This post will look at mast cells (a specific component of the immune system) and how they may influence the development of rosacea. Any products mentioned do not involve affiliate links, with all opinions and reviews being my own.
What Are Mast Cells?
Mast cells are immune cells found throughout connective tissues within the body and are responsible for several physiological processes such as the regulation of vasodilation, homeostasis within the vascular system, and immune system responses. Specifically, it is the activation and degranulation of mast cells that influence numerous physiological processes (and conditions, for example, allergies).
- Mast cell activation: The triggering of mast cells
- Mast cell degranulation: The release of pro-inflammatory chemicals from mast cells
When mast cells degranulate, they release a wide variety of chemicals, for example, histamine, cytokines, and chemokines. For more in-depth information on the role of mast cells, see this article
What Is the Connection Between Mast Cells and Rosacea?
A study funded by the National Rosacea Society discovered that mast cells could very well be the “missing link” between rosacea triggers and subsequent inflammation. The key finding was that mast cells play an explicit role in cathelicidin activation (defined as an enzyme involved in the innate immune system), which is over-produced in those suffering from rosacea. Future studies by the National Rosacea Society will aim to prove whether stabilising mast cells reduces rosacea symptoms and whether applying a mast cells stabiliser directly on the skin enables enzyme levels of ‘tryptase’ plus ‘chromotryptase’ to fall within a normal range. Another potential insight into the condition is that these two enzymes are usually high in those with rosacea.
Following up on the study mentioned above, another conducted in 2017 found a probable pathway in the inflammatory process in rosacea, unlocking further advancements in the treatment of the skin condition. Mast cells play a significant role in rosacea, with the activation of these cells occurring in the skin of sufferers. A protein present in the cell membranes defined as ‘transient receptor potential vanilloid 4’ (TRPV4), which enables the communication between cells, is closely linked to the activation of mast cells found in the skin. Another important finding in this study included a protein receptor (MRGX2) present in mast cells, which may be the causal factor of TRPV4 activation via cathelicidins. By deactivating this protein receptor (MRGX2) located in mast cells, TRPV4 could be stopped from reacting to cathelicidins. As a result, the prevention of mast cells provoking an immune response was achieved, associated with the characteristic inflammation seen in rosacea. These discoveries are potentially game-changing for future treatments, suggesting that by blocking TRPV4, prevention of inflammation associated with rosacea could be possible.

Additional Findings on Mast Cells and Rosacea
Mast cell numbers are typically higher in the skin of those with rosacea and influence other immune cells that ramp up the inflammatory response, the widening and formation of new blood vessels. Once cathelicidins have been released from the uppermost layer of the skin, mast cells are activated, resulting in inflammation. This process increases levels of cathelicidins. From this explanation alone, you can get an idea of the vicious cycle of inflammation occurring in rosacea. For more detailed information, this article is available.
Another article looks at the role of mast cells in rosacea, as well as other skin conditions. The main conclusion was that in rosacea, tryptase expression by mast cells decreased dramatically, suggesting increased degranulation of mast cells. The full article is accessible here.
Why Do Mast Cells Go Haywire?
Having looked into the definition of mast cells and their influence on rosacea, you are probably wondering what causes them to be over-activated in the first place. A variety of factors are responsible, which include:
- Certain foods (Particularly high histamine)
- Antibiotics
- Stress
- Over-exercising
- Rapid temperature fluctuations
- Fatigue
- Hormonal changes associated with the menstrual cycle
This article by ‘Healthline’ looks further into mast cells, specifically ‘mast cell activation syndrome’.
In addition to the triggers above, even though the primary cause of over-reactive mast cells is unknown, genetics probably play a role. I have not come across any studies which confirm any genetic link with mast cell-related conditions, although a comprehensive article has looked into the possibilities. As with many disorders, there is likely an intricate relationship between genetics and environmental factors, resulting in mast cells over-reacting.

Tips to Stabilise Mast Cells
In terms of stabilising mast cells, the substance often used is ‘sodium cromoglycate’. However, this medication is not clinically available for rosacea (as far as I am aware). Cromoglycate typically is prescribed for mastocytosis in tablet form.
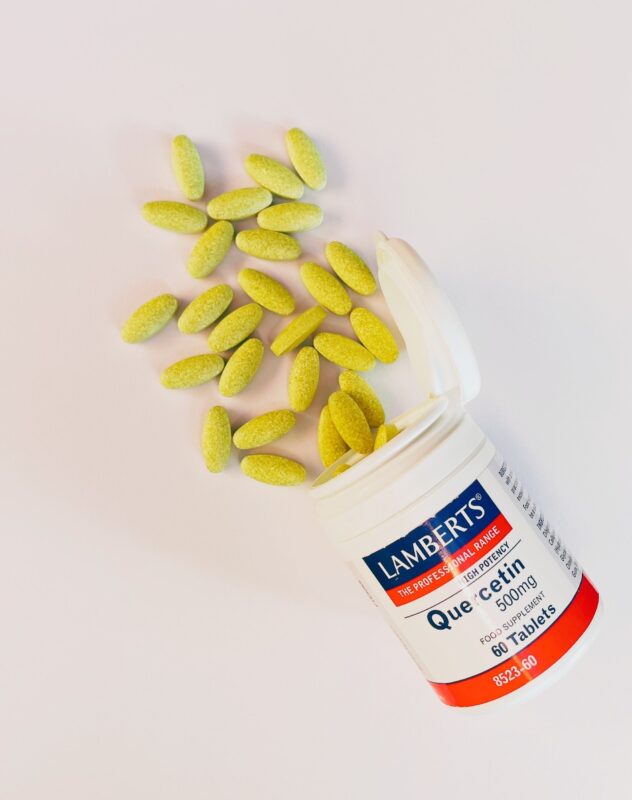
There are, however, natural methods of stabilising mast cells. A naturally occurring flavonoid ‘quercetin’, found in numerous fruits, vegetables, nuts, seeds, spices and herbs, offers anti-oxidant and anti-inflammatory properties, including the ability to stabilise mast cells. In addition to existing naturally, quercetin is available in supplement form. I have tried it over a relatively long time, in addition to eating healthily. Although many supplement brands exist, I have only tried Lamberts as recommended by the nutritionist. I felt more internally ‘stabilised’ when taking quercetin, with improved symptoms (skin and body wise). As for the product itself, there were no unwanted side effects, and although the taste took a little getting used to, it was by no means unbearable. I found the best way to take it was with food (as recommended on the packaging), specifically at breakfast. In the supplements world, debates exist as to which time of day is best to take them (morning or evening), as covered in this article. I certainly support the recommendation that taking them in the morning is more effective – and easier to remember too!
From a physiological perspective, quercetin prevents histamine, tryptase and interleukin release from mast cells. As a result, inflammation decreases as inflammatory-promoting cytokines present within mast cells are prevented from being released. For further information, this article is available.
Other foods which reduce inflammation through stabilising mast cells include:
- Watercress
- Onions
- Apples
- Peaches
- Brazil nuts
The Institute for Functional Medicine offers scientific explanations of how each of these foods stabilises mast cells.

What Difference Would Stabilising Mast Cells Make to Rosacea?
Would stabilising mast cells make any difference to rosacea symptoms? Quite possibly, “yes”, and this has been very recently (during 2020) regarded as the key focus for future rosacea treatments. As stated in ‘Dermatology Times’, Dr Webster proposed that focusing on controlling mast cells and the subsequent release of inflammatory chemicals could pave the way for more effective rosacea treatments. Being aware of high histamine foods and their impact on the skin, causing blood vessels to dilate, could also enhance the treatment of the skin condition.
From personal experience, I support the finding that stabilising mast cells goes a long way to reducing internal inflammation and improving rosacea symptoms.
Should One Potentially Be Worried About Mast Cell Disorders?
Being aware of the intricate role mast cells play within our immune system, internal inflammation and rosacea, is there a cause for concern? In terms of mast cell conditions, two key ones exist:
- Health conditions where mast cells are over-reactive: Mast Cell Activation Syndrome
- Health conditions that involve the overproduction of mast cells: Mastocytosis
Mast Cell Activation Syndrome affects a broad range of bodily systems, causing allergy-like symptoms. Symptoms can include rashes, fainting, elevated heart rate, itching, stomach cramps and dizziness.
Mastocytosis displays very similar symptoms, with sufferers being at increased risk of hives and anaphylaxis. This disorder can either be cutaneous (only involving the skin) or systemic (where several systems are affected). Further information is available here.
Given a great deal of information is available online regarding mast cells and related conditions, I wouldn’t be overly concerned about mast cell disorders as symptoms would require further investigation and a consultation with an allergist or immunologist. The purpose of this post was to raise awareness of the link between rosacea and mast cells – something which has certainly broadened my understanding, and improved overall health and rosacea, for which I am thankful.
Brissette, C. (2019) ‘What Time Of The Day Should You Take Multivitamins And Supplements - Morning Or Evening? Doctor NDTV. [Online].
Available At: https://doctor.ndtv.com/living-healthy/morning-or-night-with-food-or-without-answers-to-your-questions-about-taking-supplements-1989126#:~:text=There%20is%20debate%20about%20whether%20taking%20your%20vitamins,Washington%20Post%20%7C%20Christy%20Brissette%2C%20The%20Washington%20Post
Accessed: (23 July 2021).
Genetic and Rare Diseases Information Centre (2018) ‘Mastocytosis’. [Online].
Available At: https://rarediseases.info.nih.gov/diseases/6987/mastocytosis
Accessed: (23 July 2021).
Idahosa, C. (2015) ‘The Mast Cell Receptor Mas-Related Gene X2 (MrgX2) in Health and Disease’, University of Pennsylvania - Scholarly Commons. [Online].
Available At: https://repository.upenn.edu/cgi/viewcontent.cgi?article=1009&context=dental_theses
Accessed: (22 July 2021).
Krader, C. (2020) ‘A New Target For Rosacea Treatment: The Mast Cell’, Dermatology Times, vol. 41 (5). [Online].
Available At: https://www.dermatologytimes.com/view/new-target-rosacea-treatment-mast-cell
Accessed: (23 July 2021).
Moon, D. (2020) ‘Mast Cells: MCAS, Genetics, and Solutions’, Genetic Lifehacks. [Online].
Available At: https://www.geneticlifehacks.com/mast-cells/
Accessed: (23 July 2021).
Moyer, N. (2019) ‘Mast Cell Activation Syndrome’, Healthline. [Online].
Available At: https://www.healthline.com/health/mast-cell-activation-syndrome
Accessed: (23 July 2021).
Muto, Y., Wang, Z., Vanderberghe, M., Two, A., Gallo, R. and Nardo, A. (2014) ‘Mast Cells Are Key Mediators Of Cathelicidin Initiated Skin Inflammation In Rosacea’, Journal of Investigative Dermatology, vol. 134 (11), pp. 2728-2736. [Online].
Available At: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4199909/
Accessed: (22 July 2021).
National Rosacea Society (2014) ‘Are Mast Cells The ‘Missing Link’ For Rosacea Triggers? National Rosacea Society. [Online].
Available At: https://www.rosacea.org/blog/2014/february/are-mast-cells-the-missing-link-for-rosacea-triggers
Accessed: (21 July 2021).
The Institute for Functional Medicine ‘Mast Cell Stabilizing Foods’ [Online].
Available At: https://www.ifm.org/news-insights/fight-inflammation-stabilize-mast-cells-naturally/
Accessed: (23 July 2021).
Weng, Z., Zhang, B., Asadi, S., Sismanopoulos, N., Butcher, A., Fu, X., Katsari, A., Antoniou, C. And Theorharides, C. (2012) ‘Quercetin Is More Effective than Cromolyn in Blocking Human Mast Cell Cytokine Release and Inhibits Contact Dermatitis and Photosensitivity in Humans’, Plus One, vol. 7 (3). [Online].
Available At: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3314669/
Accessed: (23 July 2021).
Whittemore, M., Dileepan, K. and Wood, J. (2016) ‘Mast Cell: A Multi-Functional Master Cell’, Frontiers in Immunology, vol. 6 (620). [Online].
Available At: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4701915/
Accessed: (21 July 2021).

